Rachel Blair, MD
Fellow in the Division of Endocrinology, Diabetes and
Hypertension at Brigham and Women’s Hospital
PGY6
03/13/2020
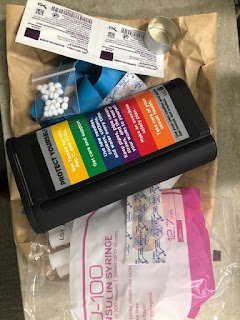
I am developing a text messaging program for women with
gestational diabetes, which is diabetes diagnosed during the 3rd
trimester of pregnancy. The program is designed to provide reminders to check
blood sugars, as well as educational and motivational messages. The program
also sends encouraging replies when women send in their blood sugars.
 |
| Screenshot showing some of the messages. |
I previously designed a novel text message library and
obtained feedback from women with gestational diabetes on the wording and
content of messages. The current stage of my project, supported by funding from
the COE for Health Policy and Management, is performing usability testing. We
are working with a vendor to create a text messaging platform with our content.
We then plan to enroll women for a two week period followed by interviews to
obtain feedback and to determine if it is easy to use and acceptable.
We have been working extensively with our vendor to
rigorously test the product before enrolling participants. We have discovered
additional scenarios during testing for which we needed to create new messages
(such as – what if someone sends in a blood sugar number unprompted?). There have been technical limitations and
we’ve come up with some creative solutions (for example, emojis cannot be
included in the program, so we are using :-) in one of our messages instead).
Next steps will include having women with gestational
diabetes use the program once all technical issues have been resolved. That
being said, recruitment will likely need to be postponed because of COVID-19.
The findings of our work creating the message library were accepted for a
poster presentation at the Endocrine Society Meeting in 2020.
I have learned that there are many unexpected roadblocks and
limitations when designing a new intervention, and it is important to be
creative when coming up with solutions for those roadblocks.